Volume
27, No. 5 – May 2014
Volume 27, No. 5
Editor: Stephen L. Seftenberg
Website:
www.CivilWarRoundTablePalmBeach.org
President’s Message
The Roundtable extends its sympathy to Dorothy Segal on the death of
her husband, David P. Segal, a long-time member. We have two exciting
programs coming up in May and June. On May 14th, Dr. Gordon Dammann, one
of the leading authorities on Civil War medicine, and his son, Douglas
Dammann will speak. Dr. Dammann is the author of several books and the
founder of the National Museum of Civil War Medicine in Frederick,
Maryland. Douglas is the Curator of the Civil War Museum of Kenosha,
Wisconsin, whose unique mission is to focus on the impact before, during
and after the Civil War on the lives of people living in Illinois,
Indiana, Iowa, Michigan, Minnesota and Wisconsin, who together sent over
750,000 men to serve in the war. We will hear about both important
Museums. On June 11th, we will have a very special "interactive"
program: Member Craig Freis will bring to the meeting actual copies (not
replicas) of the New York Times from the 1850's and 1860's. Everyone
attending will have the rare privilege of reading the newspapers and
then sharing an article with the rest of us. The print is
small, so bring a magnifying glass!
April 9, 2014 Program: Veterinary and Human Medicine
in the Civil War
Dr. Robert Altman practiced as a veterinary doctor for many years. He
broke his talk into two sections:
PART I - VETERINARY MEDICINE AND THE CIVIL WAR
At the beginning of the 19th Century the few animal
practitioners in America were uneducated or at best self-educated. Many
were farriers and farmers with animal husbandry knowledge but no medical
knowledge. At the beginning of the Civil War there were only 50 graduate
veterinarians in the entire country, all graduates of European schools.
The first veterinary school, in Lyons, France, was established in 1762.
In contrast, the first veterinary college in the U.S. was opened n 1862
in Philadelphia. The college folded because of insufficient enrollment,
before any student could graduate. The New York College of veterinary
surgeons was founded in 1857 and graduated only two students in 1867.
Sixty one years later, in 1918, when we entered World War I, only 867
graduated. The New York State Veterinary College at Cornell was
established in 1876. Its first graduate was Daniel Elmer Salmon, who
went on to discover Salmonella (which was named after him). Dr. Altman’s
father was a veterinary doctor in the Veterinary Corps, serving in
France as a 1st Lieutenant in World War I.
The start of the Civil War witnessed the formation of
dozens of cavalry regiments requiring the service of thousands of
horses. A War Department General Order in May of 1861 provided for one
veterinary sergeant for every Union cavalry regiment but said nothing of
the qualifications necessary for the post. As late as 1863 there were
only six veterinarians in the Union army. The War Department increased
the rank given to veterinary sergeants to sergeants-major and then
changed the title to veterinary surgeons, who received a salary of $75 a
month.
In 1863 Giesboro Point (now headquarters of the
Defense Intelligence Agency), was the largest Union cavalry depot with
32 stables, 6,000 stalls and a veterinary hospital that could hold 2,650
injured animals. Due to overcrowding, disease was rampant and infectious
diseases such as glanders (Pseudomonas mallei nka Burkholderia
mallei), which caused fever, a thick nasal discharge, swelling of
glands in the neck region and often death. The long incubation period of
this disease delayed its diagnosis so it spread widely. At Giesboro over
17,000 horses died in three years.
A German immigrant, Gustavus Asche-Berg was trained as a veterinarian
and practiced in the Old World for 13 years and then
practiced human medicine in the new world before joining the Union
cause in the late summer of 1861. He first joined a Pennsylvania unit as
a human surgeon, but soon switched to the 4th New Cavalry as a
veterinarian. By March of 1862 a New York cavalry unit had lost 160 of
the 780 horses originally assigned to it. With a smaller horse supply
the Confederate States established giant horse infirmaries that
emphasized rehabilitation of disabled animals rather than just buying
new ones.
It is truly ironic that in the Civil War animals were treated by
human physicians and soldiers were treated by veterinarians.
PART II - HUMAN MEDICINE DURING THE CIVIL WAR
The Civil War is considered the deadliest war of all the wars in
which the United States has participated (see table). Approximately
620,000 men (360,000 Northerners and 260,000 Southerners died in the
four year conflict. Of these approximately 110,000 Union and 94,000
Confederate men died of wounds received in battle. The rest died of
disease.
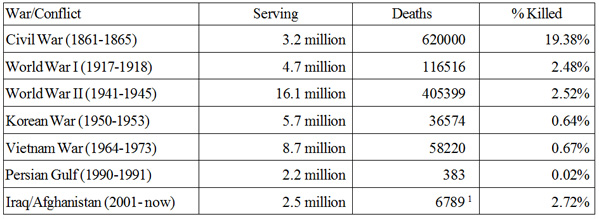
1 Through the end of 2013.
When the Civil War started in 1861, there were 85
medical schools distributed throughout 25 states, including the District
of Columbia. All had small classes. Most of the surgeons in the war were
trained during the 1840s and 1850s. This period was considered the end
of the medical Middle Ages. Little was known about what caused disease,
how to stop it from spreading, or how to cure it. Surgical techniques
ranged from barbaric to barely competent. A Civil War soldier’s chance
of NOT surviving the war was about one in five. The fallen
men were cared for by an under qualified, understaffed, and
undersupplied medical corps. However, working against incredible odds,
the Medical Corps increased in size, improved its techniques and gained
a greater understanding of medicine and disease every year the war was
fought.
 Prior
to the Civil War a physician received minimal training. Nearly all the
older doctors served as apprentices in lieu of a formal education. In
Europe four year medical schools were common, lab training was
widespread and a greater understanding of disease and infection existed.
Just before the Civil War the average medical student in the US trained
for only two years, had no clinical experience and no lab instruction.
Harvard Medical School did not own a single stethoscope or microscope
until after the war. In 1861, the Federal Army had a total of 98 Medical
officers and the Confederacy just 24. By 1865 the Union had 13,000
doctors and the Confederacy about 4,000. In addition, more than 4,000
women served as nurses in Union hospitals. By the end of the war army
doctors had treated more than 10 million wounded and sick men in just 48
months! When the war started, the US Army medical staff consisted of
only the Surgeon General, 30 surgeons and 83 assistant surgeons. Of
these, 24 resigned to go to the South and three were dropped for
disloyalty. At the end of the war in 1865, more than 11,000 doctors
served in varying capacities in the Union Army. Dr. Samuel Preston Moore
was given the rank of Colonel. To improve the quality of medical
practice, Moore insisted that every medical officer must pass an
examination set by one of his examining boards. He disliked filthy camps
and hospitals and believed in pavilion hospitals which were long wooden
buildings, well ventilated, with space for 80 to 100 beds. An important
reform was the establishment of the United States Sanitary Commission to
clean up the hospitals, speed up sanitary supplies to field hospitals,
general hospitals and hospital ships. Prior
to the Civil War a physician received minimal training. Nearly all the
older doctors served as apprentices in lieu of a formal education. In
Europe four year medical schools were common, lab training was
widespread and a greater understanding of disease and infection existed.
Just before the Civil War the average medical student in the US trained
for only two years, had no clinical experience and no lab instruction.
Harvard Medical School did not own a single stethoscope or microscope
until after the war. In 1861, the Federal Army had a total of 98 Medical
officers and the Confederacy just 24. By 1865 the Union had 13,000
doctors and the Confederacy about 4,000. In addition, more than 4,000
women served as nurses in Union hospitals. By the end of the war army
doctors had treated more than 10 million wounded and sick men in just 48
months! When the war started, the US Army medical staff consisted of
only the Surgeon General, 30 surgeons and 83 assistant surgeons. Of
these, 24 resigned to go to the South and three were dropped for
disloyalty. At the end of the war in 1865, more than 11,000 doctors
served in varying capacities in the Union Army. Dr. Samuel Preston Moore
was given the rank of Colonel. To improve the quality of medical
practice, Moore insisted that every medical officer must pass an
examination set by one of his examining boards. He disliked filthy camps
and hospitals and believed in pavilion hospitals which were long wooden
buildings, well ventilated, with space for 80 to 100 beds. An important
reform was the establishment of the United States Sanitary Commission to
clean up the hospitals, speed up sanitary supplies to field hospitals,
general hospitals and hospital ships.
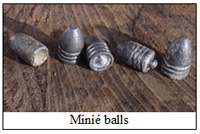 By
far the most common procedure performed in the civil war was amputation.
Almost any wound, no matter how minor, became infected. Without knowing
the cause of infection and having no medications to combat it, any wound
became infected -- mostly a Staph aureus or Strep pyogenes
bacteria. Although infection was an important reason to amputate, the
introduction of the Minié ball was
the greatest cause. The Minié ball
was invented by Claude-Étienne Minié,
an officer in the French army in the 1840s. It differed from the
standard round musket ball because of its conical shape and its hollow
base at the back of the bullet. When the trigger was pulled and the
gunpowder was ignited, the gasses formed would cause the hollow base of
the lead .58 caliber bullet to expand. The bullet would then snugly fit
into the rifled grooves of the gun barrel causing the bullet head to
spin when exiting the gun barrel giving it much greater accuracy and
increased range. This bullet caused devastating damage to both bone and
soft tissue. On entering a limb the bullet would pulverize bone and
muscle; ligaments and tendons were torn away. The wound was often 4 to 8
times larger than the base of the bullet and gangrene would inevitably
follow. Extremity wounds shattered the bone and carried dirt and
bacteria into the wound which invariably became infected. A little over
17% of extremity wounds led to amputations in both armies. Abdominal or
head wounds were almost always fatal. By
far the most common procedure performed in the civil war was amputation.
Almost any wound, no matter how minor, became infected. Without knowing
the cause of infection and having no medications to combat it, any wound
became infected -- mostly a Staph aureus or Strep pyogenes
bacteria. Although infection was an important reason to amputate, the
introduction of the Minié ball was
the greatest cause. The Minié ball
was invented by Claude-Étienne Minié,
an officer in the French army in the 1840s. It differed from the
standard round musket ball because of its conical shape and its hollow
base at the back of the bullet. When the trigger was pulled and the
gunpowder was ignited, the gasses formed would cause the hollow base of
the lead .58 caliber bullet to expand. The bullet would then snugly fit
into the rifled grooves of the gun barrel causing the bullet head to
spin when exiting the gun barrel giving it much greater accuracy and
increased range. This bullet caused devastating damage to both bone and
soft tissue. On entering a limb the bullet would pulverize bone and
muscle; ligaments and tendons were torn away. The wound was often 4 to 8
times larger than the base of the bullet and gangrene would inevitably
follow. Extremity wounds shattered the bone and carried dirt and
bacteria into the wound which invariably became infected. A little over
17% of extremity wounds led to amputations in both armies. Abdominal or
head wounds were almost always fatal.
 A
common surgeon’s tent in the field had tables or wood planks or old
doors placed on barrels where a surgeon and an assistant surgeon, often
stripped to the waist and spattered with blood, used a saw and a knife
to remove limbs very quickly, throwing the mangled limbs on a pile to be
removed later. Most amputees were administered chloroform or ether and
experienced little pain during the surgery. However, after surgery the
patient suffered a great deal of pain with no medication to offer
relief. Morphine was available but was used in limited doses. A
common surgeon’s tent in the field had tables or wood planks or old
doors placed on barrels where a surgeon and an assistant surgeon, often
stripped to the waist and spattered with blood, used a saw and a knife
to remove limbs very quickly, throwing the mangled limbs on a pile to be
removed later. Most amputees were administered chloroform or ether and
experienced little pain during the surgery. However, after surgery the
patient suffered a great deal of pain with no medication to offer
relief. Morphine was available but was used in limited doses.
Most surgeons were aware of the relationship between
cleanliness and low infection rates, but did not know how to sterilize
their instruments. Because of frequent water shortages, surgeons often
went without washing their hands or instruments thereby spreading
bacteria from one patient to another. Most infections were caused by
staph aureus and strep pyogenes. These organisms generate pus, destroy
tissue, and release toxins into the blood stream. Gangrene commonly
followed. Despite these fearful odds, 75% of the amputees survived. The
typical treatment protocol for wounds not treated by amputation was to
probe the wound for a bullet or shell or bone fragments. This was
generally done by the the surgeons unwashed hands. Bleeding blood
vessels were ligated and the wound was packed with lint. If the wound
could be closed it was sutured closed, and if not sutured the edges of
the wound were painted with iodine or other disinfectants such as
carbolic acid, bichloride of mercury or sodium hypochlorite.
Every effort was made to treat the wounded within 48
hours. Men were evacuated from the field, often several days after they
were injured because the battle was still on. They were usually carried
by litter bearers. Most primary care was administered at field hospitals
located behind the front lines. Those who survived were then transported
by unreliable and overcrowded ambulances–two wheeled carts and four
wheeled wagons and then put in two-wheeled carts and sometimes in
four-wheeled wagons, riding over rough ground without springs, making
the trip agonizing for a badly wounded patient to Army hospitals located
in nearby cities and towns.
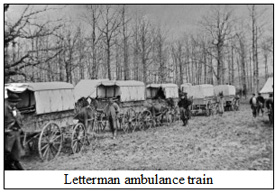 In
time for the Battle of Antietam (September 17, 1862), the Army of the
Potomac’s medical director, Dr. Jonathan Letterman, developed the
Letterman Ambulance Plan. In this system, the ambulances of a division
moved together, each ambulance under a mounted line Sergeant with two
stretcher-bearers and one driver, to collect the wounded from the field,
bring them to a field dressing station and then to the field hospital.
There were many ambulance designs though the Letterman Ambulance proved
to be the best. Most of the newer wagons had springs offering a much
smoother ride. Ambulance wagons carried both sitting and recumbent
patients. Where possible, railroads were used to evacuate wounded to
hospitals in major cities. Sadly, ward attendants and orderlies were
frequently recuperating patients, often barley able to care for
themselves. In
time for the Battle of Antietam (September 17, 1862), the Army of the
Potomac’s medical director, Dr. Jonathan Letterman, developed the
Letterman Ambulance Plan. In this system, the ambulances of a division
moved together, each ambulance under a mounted line Sergeant with two
stretcher-bearers and one driver, to collect the wounded from the field,
bring them to a field dressing station and then to the field hospital.
There were many ambulance designs though the Letterman Ambulance proved
to be the best. Most of the newer wagons had springs offering a much
smoother ride. Ambulance wagons carried both sitting and recumbent
patients. Where possible, railroads were used to evacuate wounded to
hospitals in major cities. Sadly, ward attendants and orderlies were
frequently recuperating patients, often barley able to care for
themselves.
Disease caused 60% of all deaths – half from
intestinal disorders (typhoid fever, diarrhea and dysentery), the
remainder from pneumonia and tuberculosis. Measles, chicken pox, mumps
and whooping cough were also prevalent. In the Southern areas, malaria
and yellow fever regularly swept through army camps and naval fleets. It
is estimated that 995 out of every 1,000 men contracted diarrhea. One
quarter of noncombat deaths in the Confederate Army was from typhoid
fever. A common cold often developed into pneumonia, the third leading
killer after typhoid fever and dysentery. The brilliant results from
cleaning up the Crimean War hospitals by Florence Nightingale inspired
the North to add nurses to the Army under the supervision of Dorothea
Dix. Sadly, she was disorganized, unyielding in controversy and deeply
imbued with Victorian principles, and the doctors hated her. By
contrast, Clara Barton, the founder of the American Red Cross, did an
admirable job with the wounded and sick soldiers, winning over the
doctors.
Contrary to common belief, anesthesia was used in
most amputations and other surgeries. Chloroform, ether, or a
combination of the two were used. Chloroform was preferred by far
because of ether’s explosive properties, particularly in a field
hospital where bullets or exploding cannon balls could trigger an
explosion. The most common method of administering chloroform and ether
was through a cloth or paper folded into a cone with a sponge or cloth
soaked in the anesthetic fluid in the apex. The cone was held at some
distance over the nose and mouth of the patient to allow the first few
inhalations to become diluted with air and then allow the cone to be
lowered to the nose until anesthesia was effected. The breathing of the
patient had to be monitored very carefully because there was very little
margin of error between anesthesia and death, particularly with
chloroform. Anesthetic deaths were surprisingly low considering the
crude means of administration. With chloroform anesthetic deaths
occurred in 5.4 per thousand cases, and with ether 3.0 deaths per
thousand, but chloroform was preferred because of ether’s tendency to
explode.
In the Southern army, where chloroform was scarce,
Surgeon J. J. Chisolm devised a cylinder 2½ inches long and one inch wide with a perforated plate on one of its
surfaces and a cover with nose pieces. Chloroform could then be poured
thru the perforated plate onto a sponge or cotton and inhaled by the
patient thru the nose pieces. Both chloroform and ether evaporated in
the air quickly. This method was a vast improvement over the open drip
technique where much of the anesthetic liquids would evaporate and be
lost, particularly when the surgery was done in the field.
inches long and one inch wide with a perforated plate on one of its
surfaces and a cover with nose pieces. Chloroform could then be poured
thru the perforated plate onto a sponge or cotton and inhaled by the
patient thru the nose pieces. Both chloroform and ether evaporated in
the air quickly. This method was a vast improvement over the open drip
technique where much of the anesthetic liquids would evaporate and be
lost, particularly when the surgery was done in the field.
Dr. Altman closed his talk by saying, "It amazes me
how in those chaotic times record keeping was as efficient and complete
as it was."
After a question and answer session, Dr. Altman received a
well-deserved round of applause for his efforts.
Last changed: 05/10/14
Home
About News
Newsletters
Calendar
Memories
Links Join
|

